What is Polio
The Virus
Polio is caused by a human enterovirus called the poliovirus. Polio can interact in its host in two ways:
Infection not including the central nervous system, which causes a minor illness with mild symptoms
Infection including the central nervous system, which may cause paralysis
Less than 1% of poliovirus infections result in paralysis. The virus is most often spread by the faecal-oral route. Poliovirus enters through the mouth and multiplies in the intestine. Infected individuals shed poliovirus into the environment for several weeks, where it can spread rapidly through a community, especially in areas of poor sanitation.
The poliovirus consists of an RNA genome enclosed in a protein shell called a capsid. There are three serotypes of wild poliovirus type 1, type 2, and type 3 each with a slightly different capsid protein. Immunity to one serotype does not give confer immunity to the other two. Outbreaks of poliovirus were largely unknown prior to the 20th century. However, with improved sanitation in the 20th century, the average age at which individuals were exposed to poliovirus increased. With progressively declining protection from maternal antibodies, poliovirus infection increasingly resulted in paralysis.
Type 2 poliovirus was declared eradicated in September 2015, with the last virus detected in India in 1999. Type 3 wild poliovirus has not been detected anywhere in the world since November 2012.
Testing for polioviruses
All cases of acute flaccid paralysis (AFP) among children under fifteen years of age are reported and tested for wild poliovirus or vaccine-derived polioviruses within 48 hours of onset. AFP is caused by a range of factors. The Global Polio Laboratory Network tests upwards of 100,000 AFP samples a year, of which a very small portion are positive for poliovirus.
Who is at risk?
Polio can strike at any age, but it mainly affects children under five years old.
Transmission:
Polio is spread through person-to-person contact. When a child is infected with wild poliovirus, the virus enters the body through the mouth and multiplies in the intestine. It is then shed into the environment through the faeces where it can spread rapidly through a community, especially in situations of poor hygiene and sanitation. If a sufficient number of children are fully immunized against polio, the virus is unable to find susceptible children to infect, and dies out.
Young children who are not yet toilet-trained are a ready source of transmission, regardless of their environment. Polio can be spread when food or drink is contaminated by faeces. There is also evidence that flies can passively transfer poliovirus from faeces to food.
Most people infected with the poliovirus have no signs of illness and are never aware they have been infected. These symptomless people carry the virus in their intestines and can “silently” spread the infection to thousands of others before the first case of polio paralysis emerges.
For this reason, WHO considers a single confirmed case of polio paralysis to be evidence of an epidemic – particularly in countries where very few cases occur.
Symptoms:
Most infected people (90%) have no symptoms or very mild symptoms and usually go unrecognized. In others, initial symptoms include fever, fatigue, headache, vomiting, stiffness in the neck and pain in the limbs.
Acute flaccid paralysis (AFP)
One in 200 infections leads to irreversible paralysis, usually in the legs. This is caused by the virus entering the blood stream and invading the central nervous system. As it multiplies, the virus destroys the nerve cells that activate muscles. The affected muscles are no longer functional and the limb becomes floppy and lifeless – a condition known as acute flaccid paralysis (AFP).
All cases of acute flaccid paralysis (AFP) among children under fifteen years of age are reported and tested for poliovirus within 48 hours of onset.
Bulbar polio
More extensive paralysis, involving the trunk and muscles of the thorax and abdomen, can result in quadriplegia. In the most severe cases (bulbar polio), poliovirus attacks the nerve cells of the brain stem, reducing breathing capacity and causing difficulty in swallowing and speaking. Among those paralysed, 5% to 10% die when their breathing muscles become immobilized.
In the 1940s and 1950s, people with bulbar polio were immobilized inside “iron lungs” – huge metal cylinders that operated like a pair of bellows to regulate their breathing and keep them alive. Today, the iron lung has largely been replaced by the positive pressure ventilator, but it is still in use
Post-polio syndrome:
Around 40% of people who survive paralytic polio may develop additional symptoms 15–40 years after the original illness. These symptoms – called post-polio syndrome – include new progressive muscle weakness, severe fatigue and pain in the muscles and joints.
Risk factors for paralysis:
No one knows why only a small percentage of infections lead to paralysis. Several key risk factors have been identified as increasing the likelihood of paralysis in a person infected with polio. These include:
Treatment and prevention:
There is no cure for polio, only treatment to alleviate the symptoms. Heat and physical therapy is used to stimulate the muscles and antispasmodic drugs are given to relax the muscles. While this can improve mobility, it cannot reverse permanent polio paralysis.
Polio can be prevented through immunization. Polio vaccine, given multiple times, almost always protects a child for life.
History of Polio
In the early 20th century, polio was one of the most feared diseases in industrialized countries, paralyzing hundreds of thousands of children every year. Soon after the introduction of effective vaccines in the 1950s and 1960s however, polio was brought under control and practically eliminated as a public health problem in these countries.
It took somewhat longer for polio to be recognized as a major problem in developing countries. Lameness surveys during the 1970s revealed that the disease was also prevalent in developing countries. As a result, during the 1970s routine immunization was introduced worldwide as part of national immunization programmes, helping to control the disease in many developing countries.
In 1988, when the Global Polio Eradication Initiative began, polio paralysed more than 1000 children worldwide every day. Since then, more than 2.5 billion children have been immunized against polio thanks to the cooperation of more than 200 countries and 20 million volunteers, backed by an international investment of more than US$ 11 billion.
There are now only 2 countries fighting wild polio transmission and global incidence of polio cases has decreased by 99.9%.
There has also been success in eradicating certain strains of the virus; of the three types of wild polioviruses (WPVs), the last case of type 2 was reported in 1999 and its eradication was declared in September 2015; the most recent case of type 3 dates to November 2012.
However, tackling the last 1% of polio cases has still proved to be difficult. Conflict, political instability, hard-to-reach populations, and poor infrastructure continue to pose challenges to eradicating the disease. Each country offers a unique set of challenges which require local solutions. Thus, in 2013 the Global Polio Eradication Initiative launched its most comprehensive and ambitious plan for completely eradicating polio. It is an all-encompassing strategic plan that clearly outlines measures for eliminating polio in its last strongholds and for maintaining a polio-free world.
Use this interactive timeline above to trace the history of polio from 1580 B.C. to the present.
The Vaccines
The development of effective vaccines to prevent paralytic polio was one of the major medical breakthroughs of the 20th century. The Global Polio Eradication Initiative uses two types of vaccine to stop polio transmission – inactivated polio vaccine (IPV) and oral polio vaccine (OPV).
If enough people in a community are immunized against polio, the virus will be deprived of susceptible hosts and will die out. High levels of vaccination coverage must be maintained to stop transmission and prevent outbreaks occurring. The Global Polio Eradication Initiative is constantly assessing the optimal use of the different types of vaccine to prevent paralytic polio and stop poliovirus transmission in different areas of the world.
OPV – Oral poliovirus vaccine
Oral poliovirus vaccines (OPV) are the predominant vaccine used in the fight to eradicate polio. There are different types of oral poliovirus vaccine, which may contain one, a combination of two, or all three different serotypes of attenuated vaccine. Each has their own advantages and disadvantages over the others.
The attenuated poliovirus(es) contained in OPV are able to replicate effectively in the intestine, but around 10,000 times less able to enter the central nervous system than the wild virus. This enables individuals to mount an immune response against the virus. Virtually all countries which have eradicated polio used OPV to interrupt person to person transmission of the virus.
Advantages:
OPVs are all inexpensive (US $0.12-$0.18 for countries procuring through UNICEF in 2016).
OPVs are safe and effective and offer long lasting protection against the serotype(s) which they target. OPV stimulates good mucosal immunity, which is why it is so effective at interrupting transmission of the virus.
OPVs are administered orally and do not require health professionals or sterile needle syringes. As such, OPVs are easy to administer in mass vaccination campaigns.
For several weeks after vaccination the vaccine virus replicates in the intestine, is excreted and can be spread to others in close contact. This means that in areas with poor hygiene and sanitation, immunization with OPV can result in ‘passive’ immunization of people who have not been vaccinated.
Disadvantages:
OPV is extremely safe and effective. However, in extremely rare cases (at a rate of approximately 2 to 4 events per 1 million births [1]) the live attenuated vaccine-virus in OPV can cause paralysis. In some cases, it is believed that this may be triggered by an immunodeficiency. The extremely low risk of vaccine-associated paralytic poliomyelitis (VAPP) is well accepted by most public health programmes.
Very rarely, when there is insufficient coverage in a community the vaccine-virus may be able to circulate, mutate and, over the course of 12 to 18 months, reacquire neurovirulence. This is known as a circulating vaccine-derived poliovirus.
Monovalent oral poliovirus vaccine (mOPV)
Prior to the development of tOPV, monovalent OPVs (mOPVs) were developed in the early 1950s, but largely dropped out of use upon the adoption of tOPV. It was not available at the time of the founding of GPEI in 1988. Monovalent oral polio vaccines confer immunity to just one of the three serotypes of OPV. They are more successful in conferring immunity to the serotype targeted than tOPV, but do not provide protection to the other two types.
Monovalent OPVs for type 1 (mOPV1) and type 3 (mOPV3) poliovirus were licensed again in 2005, thanks to successful action taken by the GPEI. They elicit the best immune response against the serotype they target of all the vaccines.
Monovalent OPV type 2 (mOPV2) has been stockpiled in the event of a cVDPV2 outbreak.
Bivalent oral poliovirus vaccine (bOPV)
Following April 2016, the trivalent oral poliovirus vaccine was replaced with the bivalent oral poliovirus vaccine (bOPV) in routine immunization around the world. Bivalent OPV contains only attenuated virus of serotypes 1 and 3, in the same number as in the trivalent vaccine.
Bivalent OPV elicits a better immune response against poliovirus types 1 and 3 than trivalent OPV, but does not give immunity against serotype 2. As well as in routine immunization, bOPV will be used for outbreak response against poliovirus types 1 and 3 outbreaks.
Trivalent oral poliovirus vaccine (tOPV)
Prior to April 2016, the trivalent oral poliovirus vaccine (tOPV) was the predominant vaccine used for routine immunization against poliovirus. Developed in the 1950s by Albert Sabin, tOPV consists of a mixture of live, attenuated polioviruses of all three serotypes. Also called the ‘Sabin vaccine’, tOPV is inexpensive and effective, and offers long lasting protection to all three serotypes of poliovirus.
The trivalent vaccine was withdrawn in April 2016 and replaced with the bivalent oral poliovirus vaccine (bOPV), which contains only attenuated virus of types 1 and 3. This is because continued use of tOPV threatened to continue seeding new type 2 circulating vaccine-derived polioviruses (cVDPV2), despite the wild type 2 virus being eradicated in 1999.
IPV- Inactivated poliovirus vaccine
Inactivated polio vaccine (IPV) was developed in 1955 by Dr Jonas Salk. Also called the Salk vaccine IPV consists of inactivated (killed) poliovirus strains of all three poliovirus types. IPV is given by intramuscular or intradermal injection and needs to be administered by a trained health worker. IVP produces antibodies in the blood to all three types of poliovirus. In the event of infection, these antibodies prevent the spread of the virus to the central nervous system and protect against paralysis.
Advantages
As IPV is not a ‘live’ vaccine, it carries no risk of VAPP.
IPV triggers an excellent protective immune response in most people.
Disadvantages
IPV induces very low levels of immunity in the intestine. As a result, when a person immunized with IPV is infected with wild poliovirus, the virus can still multiply inside the intestines and be shed in the faeces, risking continued circulation.
IPV is over five times more expensive than OPV. Administering the vaccine requires trained health workers, as well as sterile injection equipment and procedures.
Safety
IPV is one of the safest vaccines in use. No serious systemic adverse reactions have been shown to follow vaccination.
Efficacy
IPV is highly effective in preventing paralytic disease caused by all three types of poliovirus.
Recommended use
An increasing number of industrialized, polio-free countries are using IPV as the vaccine of choice. This is because the risk of paralytic polio associated with continued routine use of OPV is deemed greater than the risk of imported wild virus.
However, as IPV does not stop transmission of the virus, OPV is used wherever a polio outbreak needs to be contained, even in countries which rely exclusively on IPV for their routine immunization programme.
Once polio has been eradicated, use of all OPV will need to be stopped to prevent re-establishment of transmission due to VDPVs.
The Communities
Health Workers are the key
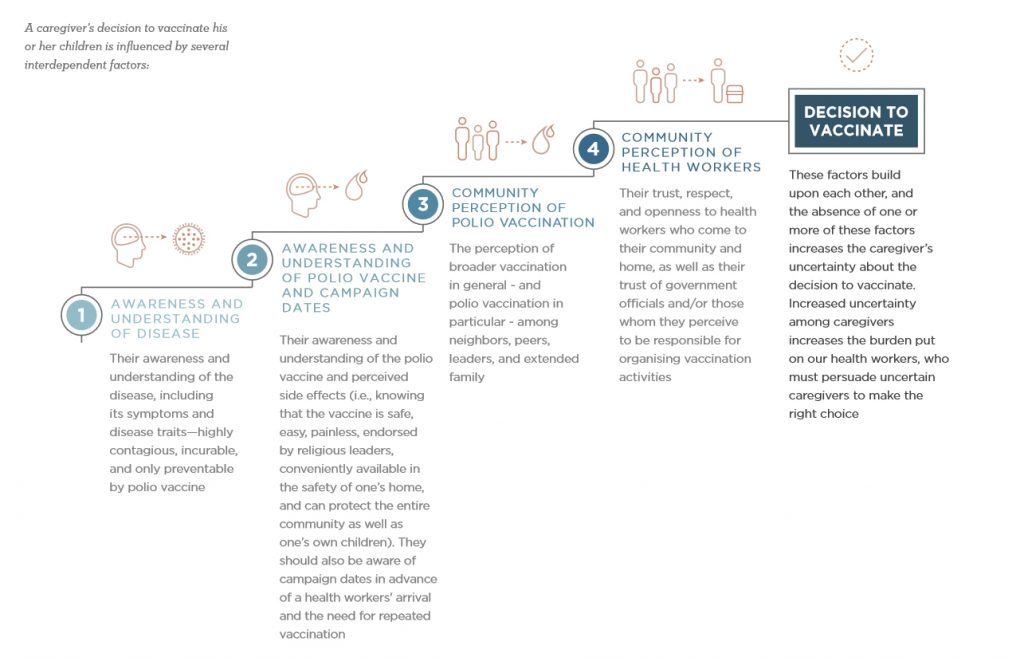
When polio was widespread, communication strategies often used what is known as risk communication, targeting individual caregivers with facts about polio and polio vaccination to inform caregivers and educate communities about the need to protect and vaccinate children. As the virus’ hold has shrunk to very limited parts of the world, communications has evolved to address the dynamic perceptions and social norms that deter caregivers in the remaining 1% of the world from vaccinating their children.
The Global Polio Eradication Initiative’s shift to ‘social norm communication’ is led by UNICEF and grounded in recent polling research on populations affected by polio in endemic and outbreak contexts, and their responses to polio eradication efforts. Primarily, this research shows that families in high-risk areas are discouraged from vaccinating by the prevalent social norms. Communication strategies therefore aim to shift those norms, much as smoking has been shifted from the norm in many countries.
The eradication of polio depends on the success of polio programme health workers (e.g., community health workers, social mobilisers, vaccinators). Their success in the field revolves around a single pivotal moment: the short, interpersonal interaction between health workers and caregivers, or ‘the knock’ on the door.
The Communities
A caregiver’s decision does not exist in isolation. It is both a personal decision, and a consideration of familial and community views about the act of vaccination itself.
Is it celebrated or discouraged?
Does the community respect the role of health workers?
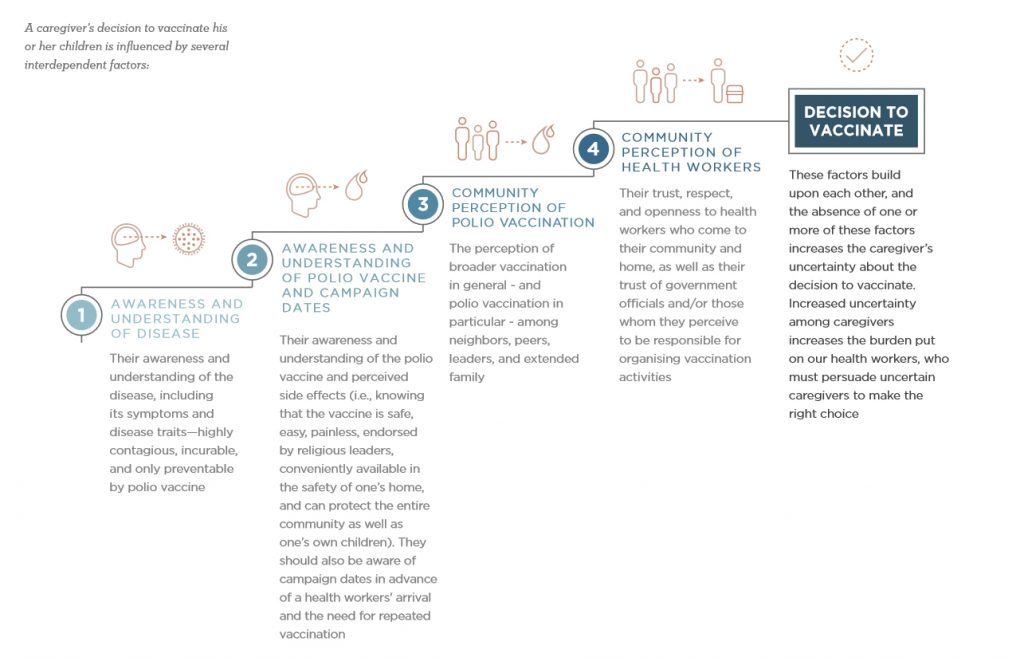
Community engagement does not just happen during vaccination days. It is an ongoing conversation with the community that requires an iterative loop of listening and responding.
The GPEI Community Engagement Strategy considers three main phases:
Before the Knock – Pre-campaign awareness and community mobilization
The Interaction – Supporting interpersonal communication and training so that the interaction at the door is the most effective it can be.
After the Knock – Building toward constant improvement and increased levels of trust, seeking caregiver feedback is critical.

UNICEF’s goal is to use this strategy to increase the uptake of valuable, life-saving services, such as the polio vaccine. To do this, UNICEF needs to work with communities to build social demand for vaccination, and present the health workers as trustworthy, admirable, compassionate, helpful, and competent across all of the touch points and caregiver-targeted messages.